
Introduction: The Adult Acne Dilemma
For millions of adults, the reflection in the mirror presents a frustrating paradox: the persistence of a skin condition widely believed to be the exclusive domain of adolescence. The notion that acne is a rite of passage one simply "outgrows" is a pervasive misconception that leaves many feeling isolated and perplexed by breakouts that continue well into their 20s, 30s, 40s, and beyond. This experience is not an anomaly; it is a significant and growing clinical phenomenon.
The landscape of acne is shifting. Over the past decade, the average age of individuals seeking treatment for acne has risen from 20.5 to 26.5 years, a clear indicator that this is no longer just a teenage problem. Globally, acne vulgaris affects an estimated 9.4% of the population, and its prevalence remains remarkably high in adulthood, impacting 19.3% of adults between the ages of 25 and 39. This trend is not merely a statistical curiosity; it is a clinical signal pointing towards the increasing influence of modern lifestyle factors—such as chronic stress, environmental pollution, and complex dietary patterns—on a more mature hormonal and physiological system, setting adult acne apart from its adolescent counterpart.
The burden of adult acne is disproportionately carried by women. Data reveals prevalence rates as high as 50.9% in women aged 20-29, persisting at 33% for those in their 30s and 25% in their 40s. Consequently, female patients account for nearly two-thirds of all dermatological visits for acne, with up to 15% of all adult women affected by the condition.
Crucially, the impact of adult acne extends far beyond skin deep. It is a recognized medical condition with profound psychosocial consequences. Studies have linked acne to a higher risk of depression, anxiety, diminished self-esteem, and social withdrawal. Individuals with acne report feeling excluded, rejected, and stigmatized, with many experiencing fatigue, sleep difficulties, and a significant negative impact on their overall quality of life. The treatment of acne is not just a cosmetic endeavor; it is a therapeutic intervention that has been shown to reduce symptoms of depression and improve mental well-being.
This guide serves as a comprehensive, evidence-based roadmap to understanding and managing adult acne. It will deconstruct the unique characteristics of adult breakouts, explore the complex web of causes, provide a detailed analysis of the full spectrum of treatment options—from over-the-counter solutions to advanced dermatological procedures—and offer a practical blueprint for long-term management and a return to clear, resilient skin.
Understanding Adult Acne: More Than Just a Pimple
To effectively manage adult acne, one must first recognize it as a distinct clinical entity with unique characteristics that differentiate it from the more commonly understood adolescent form. The skin of an adult is not the same as that of a teenager, and neither is the acne that affects it.
Adult vs. Adolescent Acne: A Tale of Two Skins
The differences between adult and adolescent acne are fundamental, encompassing their clinical presentation, typical location, the underlying condition of the skin, and the primary factors that drive them.
- Clinical Presentation: Adult acne is predominantly inflammatory, characterized by lesions that are often red, sensitive, and tender. Breakouts tend to manifest as deeper, more painful bumps, nodules, and cystic lesions.
- Location: While adolescent acne frequently populates the T-zone (forehead, nose, and chin), adult acne has a characteristic distribution along the lower face. It most commonly appears in the "U-zone"—the area around the mouth, the chin, and the jawline.
- Skin Condition: The canvas on which adult acne appears is markedly different. Adult skin is less resilient, with a slower rate of cellular turnover. It is also more likely to be combination or dry, sensitive, and prone to dehydration, whereas teenage skin is typically oilier.
- Healing and Scarring: The sluggish cell turnover rate in adult skin has significant consequences for healing. Post-inflammatory hyperpigmentation (PIH)—the dark spots left behind after a blemish heals—and permanent scarring are more pronounced and persistent concerns for adults.
The following table provides a clear, at-a-glance summary of these critical distinctions.
|
Feature |
Adolescent Acne |
Adult Acne |
|
Typical Age |
12-24 years |
25+ years |
|
Primary Location |
T-zone (forehead, nose), chest, back |
U-zone (lower face, jawline, chin, around mouth) |
|
Common Lesion Types |
Mix of blackheads, whiteheads, papules, and pustules |
Deeper, inflammatory, and often painful papules, nodules, and cysts |
|
Underlying Skin Condition |
Oily, resilient, high cell turnover rate |
Less resilient, slower cell turnover, often dry, sensitive, or dehydrated |
|
Primary Drivers |
Pubertal surge in androgen hormones |
Hormonal fluctuations (menstrual cycle, PCOS), chronic stress, lifestyle factors |
|
Healing/Scarring Risk |
Faster healing, lower risk of prolonged marks |
Slower healing, higher risk of persistent post-inflammatory hyperpigmentation and scarring |
The Anatomy of a Breakout: The Four Pillars of Acne Pathophysiology
Regardless of age, all forms of acne vulgaris are rooted in a complex interplay of four key physiological processes that occur within the pilosebaceous unit (the hair follicle and its associated sebaceous gland).
- Excess Sebum Production: The sebaceous glands produce an oily, waxy substance called sebum. In acne-prone individuals, these glands become overactive.
- Follicular Hyperkeratinization: Dead skin cells inside the hair follicle do not shed properly. Instead, they clump together and mix with the excess sebum, forming a plug that blocks the pore.
- Cutibacterium acnes (C. acnes) Proliferation: This bacterium, a normal resident of the skin, thrives in the clogged follicle and multiplies rapidly.
- Inflammation: The body's immune system recognizes the overgrowth of C. acnes and launches an inflammatory response, resulting in the redness, swelling, and pain characteristic of an inflammatory pimple.
Identifying Your Acne: A Clinical Guide to Lesions
Accurately identifying the type of lesions present is the first step in determining the severity of the condition. Acne lesions are broadly categorized as either non-inflammatory or inflammatory.1
Non-Inflammatory Lesions (Comedonal Acne)
- Whiteheads (Closed Comedones): These occur when the follicle is completely blocked, trapping sebum, bacteria, and dead skin cells beneath the skin's surface.
- Blackheads (Open Comedones): In this case, the pore remains open to the air. The trapped mixture of sebum and skin cells is exposed to oxygen, which causes it to oxidize and turn a dark color. This dark spot is due to oxidized pigment (melanin) and lipids, not dirt.
Inflammatory Lesions
- Papules: When the wall of a hair follicle breaks, it allows bacteria and sebum to spill into the surrounding skin tissue, creating small, solid, red, and tender bumps.
- Pustules: These are what most people picture when they think of a "pimple." They are similar to papules but are filled with yellowish fluid (pus).
- Nodules: These are a severe form of inflammatory acne. They form as large, hard, painful lumps deep within the skin and often lead to scarring.2
- Cysts: Representing the most severe form of acne, cysts are large, soft, deep, painful, pus-filled lesions that carry a very high risk of causing permanent scarring.
Navigating the complexities of why you are still breaking out can be a persistent challenge, extending far beyond the teenage years. Understanding the triggers behind these breakouts is the first crucial step toward achieving lasting clarity. For a comprehensive guide to adult acne, Sylvaia.com offers expertly crafted articles that delve into the science of your skin, helping you identify the root causes and build an effective routine for a clearer complexion.
The Root Causes: Unraveling the "Why" Behind Your Breakouts
Adult acne is a multifactorial condition, meaning it rarely stems from a single cause.3 It arises from a complex interplay of internal predispositions and external triggers. The key to successful treatment lies in identifying an individual's primary driver, such as an underlying hormonal sensitivity, and understanding how it is influenced by secondary exacerbators, like stress or diet.
The Hormonal Connection: The Primary Driver in Adult Women
For the majority of adult women, hormones are the central orchestrator of acne breakouts.
- The Role of Androgens: Androgens, often referred to as "male" hormones like testosterone, are the primary hormonal regulators of sebum production. In many women with adult acne, the problem is not an abnormally high level of androgens, but rather a heightened sensitivity of their sebaceous glands to normal circulating levels of these hormones.4
- The Menstrual Cycle: The cyclical nature of breakouts is a direct reflection of hormonal fluctuations.5 In the week leading up to menstruation, estrogen and progesterone levels drop, while testosterone levels remain relatively stable. This relative increase in androgenic influence can trigger a surge in sebum production.
- Systemic Conditions: In some cases, adult acne is a visible sign of an underlying endocrine disorder. The most common of these is Polycystic Ovary Syndrome (PCOS), a condition that often presents with acne, hirsutism (excess facial and body hair), and irregular menstrual cycles.6
- Major Life Stages: Significant hormonal shifts throughout a woman's life can also trigger or worsen acne, including pregnancy, perimenopause, and menopause.7
The Stress-Acne Axis: How Your Mind Affects Your Skin
The link between stress and acne is a well-documented physiological reality.
- The Physiological Pathway: When the body perceives stress, it activates the Hypothalamus-Pituitary-Adrenal (HPA) axis, triggering the release of cortisol.
- Cortisol's Impact: Both cortisol and other stress hormones have been shown to directly bind to receptors in the skin's sebaceous glands, stimulating them to produce more oil. Furthermore, stress promotes a state of systemic inflammation, which can amplify the immune response within a clogged pore.
- The Vicious Cycle: The relationship is often bidirectional, creating an "acne-stress cycle." An initial period of stress can trigger a flare-up.8 The appearance of these blemishes then becomes a new source of psychological distress, elevating stress levels and perpetuating the cycle.9
The Genetic Blueprint: Is Acne in Your DNA?
The foundation for acne susceptibility is often laid in one's genetic code.10 A strong family history is one of the most reliable predictors of whether an individual will experience acne.11
- Heritability: Large-scale twin studies have provided compelling evidence for a strong genetic basis, with one UK study concluding that genetics account for as much as 81% of the variance in acne prevalence.12
- Genetic Mechanisms: There is no single "acne gene." Instead, multiple genes are thought to influence factors like overactive sebaceous glands, a robust inflammatory response, or an abnormal pattern of skin cell shedding.
- Validation: Understanding the powerful genetic component of acne can be validating. It underscores the fact that acne is a medical condition rooted in biology, not a reflection of personal hygiene or lifestyle failings.
The Diet Debate: Fueling the Fire?
A growing body of scientific evidence suggests that certain dietary patterns can influence or exacerbate breakouts in susceptible individuals.13
- High-Glycemic Index (GI) Foods: High-GI foods (refined carbohydrates like white bread, sugary drinks, pastries) cause a quick spike in blood sugar and insulin. This state of hyperinsulinemia stimulates the production of insulin-like growth factor 1 (IGF-1), a hormone that can increase androgen production and directly stimulate sebaceous glands.
- Dairy Consumption: Several studies have found a correlation between the consumption of cow's milk and acne, with skim milk showing the strongest association. One large study of adult women found that those who drank two or more glasses of skim milk per day were 44% more likely to have acne.14 The leading theory is that hormones and growth factors naturally present in milk can disrupt the body's endocrine balance.
- Nuance is Key: It is critical to note that dietary triggers are highly individual. Not everyone who consumes dairy or high-GI foods will develop acne.
External Aggressors: The Impact of Your Environment
- Pollution-Induced Acne: Microscopic pollutants in urban environments can settle on the skin, physically clogging pores.15 More insidiously, they generate free radicals that cause oxidative stress.
- Barrier Dysfunction: This oxidative stress attacks and weakens the skin's protective barrier, leading to dryness, increased sensitivity, an overproduction of oil to compensate, and increased inflammation.
- Chloracne: In rare cases, systemic exposure to certain industrial chemicals can cause a severe variant of acne called chloracne.16
Skincare and Cosmetics: Unwitting Accomplices?
Acne cosmetica is a term for acne caused or exacerbated by skincare, makeup, or hair care products containing pore-clogging, or "comedogenic," ingredients.17 The following table lists some common comedogenic ingredients to watch for.
|
Ingredient Category |
Common Comedogenic Examples |
Found In |
|
Oils & Butters |
Coconut Oil, Cocoa Butter, Almond Oil, Soybean Oil, Palm Oil |
Moisturizers, cleansers, "natural" skincare, foundations |
|
Waxes |
Beeswax, Candelilla Wax, Carnauba Wax |
Balms, thick creams, concealers, foundations |
|
Fatty Acids & Esters |
Isopropyl Myristate, Isopropyl Palmitate, Butyl Stearate |
Moisturizers, foundations, primers, some acne medications |
|
Lanolins |
Lanolin, Acetylated Lanolin, Ethoxylated Lanolin |
Rich creams, balms, lip products |
|
Thickeners & Emulsifiers |
Carrageenan, Ceteareth-20 (with Cetearyl Alcohol) |
Lotions, creams, serums |
|
Silicones |
Dimethicone (in some cases, if not properly cleansed) |
Primers, sunscreens, foundations |
|
Pigments |
D&C Red dyes (derived from coal tar) |
Blushes, bronzers, lipsticks |
|
Miscellaneous |
Algae Extract, Coal Tar, Colloidal Sulfur |
Serums, masks, some therapeutic products |
A Strategic Approach to Treatment: From OTC to Advanced Dermatology
The modern approach to managing adult acne, informed by the 2024 clinical practice guidelines from the American Academy of Dermatology (AAD), emphasizes the use of combination therapies that target multiple aspects of acne pathophysiology simultaneously.18 It also prioritizes antibiotic stewardship—the judicious use of antibiotics—to combat bacterial resistance.19
Building Your First Line of Defense: Over-the-Counter (OTC) Solutions
For mild adult acne, over-the-counter products are the appropriate first line of defense.
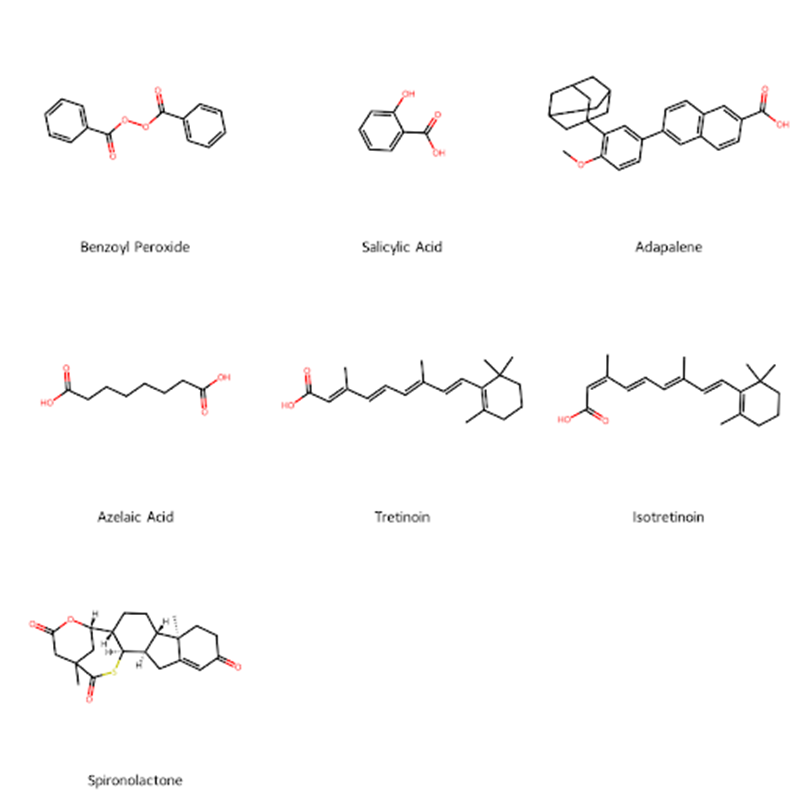
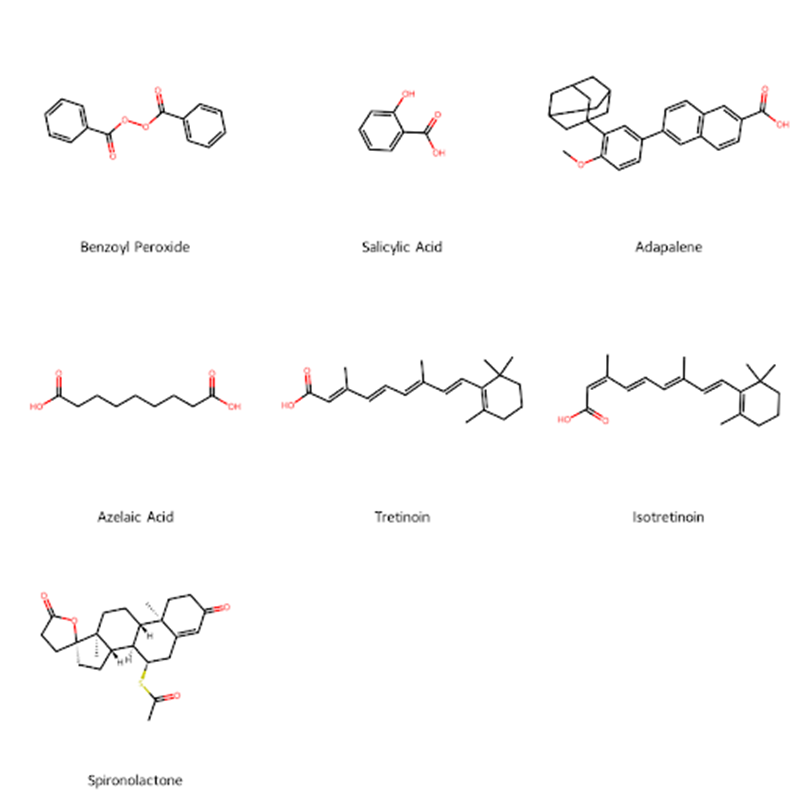
- Benzoyl Peroxide (BPO): This is a cornerstone of OTC treatment. It works primarily as a potent antimicrobial agent that kills the C. acnes bacteria. Lower concentrations (2.5% or 5%) are often just as effective as higher ones but with a significantly lower risk of irritation.
- Salicylic Acid (BHA): Salicylic acid is a beta-hydroxy acid, meaning it is oil-soluble.20 This property allows it to penetrate deep into the pores to dissolve the clogs of sebum and dead skin cells. It is most effective for non-inflammatory comedonal acne.
- Adapalene 0.1% Gel: Adapalene is a type of retinoid, a class of compounds derived from vitamin A. It is the only retinoid available OTC. Retinoids work by normalizing the process of skin cell turnover within the follicle, which prevents the formation of the initial plug.21
- Azelaic Acid: This naturally occurring acid possesses antibacterial properties, helps to reduce inflammation, and can also help fade post-inflammatory hyperpigmentation.
|
Ingredient |
Mechanism of Action |
Best For (Lesion Type) |
Potential Side Effects |
|
Benzoyl Peroxide |
Antimicrobial; kills C. acnes bacteria |
Inflammatory acne (papules, pustules) |
Dryness, peeling, redness, irritation; can bleach fabric |
|
Salicylic Acid (BHA) |
Oil-soluble exfoliant; dissolves clogs inside pores |
Non-inflammatory acne (blackheads, whiteheads) |
Mild stinging, skin irritation, dryness |
|
Adapalene 0.1% Gel (Retinoid) |
Normalizes skin cell turnover; anti-inflammatory |
All mild acne, especially comedones; preventative care |
Dryness, scaling, initial "purging" period; sun sensitivity |
|
Azelaic Acid |
Antibacterial; anti-inflammatory; fades post-acne marks |
Mild inflammatory acne; post-inflammatory hyperpigmentation |
Mild irritation, potential for skin lightening |
Escalating Care: Prescription Medications (AAD Guideline-Informed)
When OTC treatments are insufficient after two to three months, or for moderate to severe acne, it is time to consult a dermatologist.
Topical Therapies
- Prescription Retinoids:Tretinoin and tazarotene are more potent versions of the retinoid class of drugs.
- Topical Antibiotics: Clindamycin and erythromycin reduce C. acnes bacteria. A critical point in the 2024 AAD guidelines is that topical antibiotics should never be used as a standalone therapy. They should always be used in combination with benzoyl peroxide to prevent resistance.
- Other Topicals: Advanced
agents include clascoterone, a novel topical anti-androgen, and
higher concentrations of azelaic acid.
Systemic (Oral)
Therapies
For more widespread, severe, or treatment-resistant acne,
oral medications are necessary.
- Oral Antibiotics: These are indicated for moderate to severe inflammatory acne. The tetracycline class of antibiotics, including doxycycline, minocycline, and sarecycline, are preferred. To practice good antibiotic stewardship, their use should be limited to the shortest effective duration, typically three to four months.
- Hormonal Agents (For Women): This
category is a cornerstone for managing adult female acne.
- Combined Oral Contraceptives (OCPs): Several birth control pills are FDA-approved for acne. They work by decreasing circulating androgens, which in turn reduces sebum production.
- Spironolactone: This medication functions as an anti-androgen. It works by blocking androgen receptors on the sebaceous glands, preventing testosterone from stimulating oil production. It is highly effective for hormonally-driven acne on the lower face and jawline.
- Isotretinoin: Formerly known as Accutane, oral isotretinoin is a potent vitamin A derivative reserved for the most severe cases of acne. It is the only medication that addresses all four pillars of acne pathophysiology, often leading to long-term remission. However, it carries significant side effects, including a severe risk of birth defects, requiring all patients to enroll in the strict FDA-mandated iPLEDGE risk management program.
In-Office Procedures: Targeted Professional Interventions
Dermatologists can perform a variety of in-office procedures to accelerate clearing and address long-term consequences like scarring.
For Active Acne
- Corticosteroid Injections: For large, inflamed nodules or cysts, a dilute corticosteroid can be injected directly into the lesion, providing rapid reduction in inflammation and pain within 24-48 hours.
- Comedo Extraction: A dermatologist can use sterile instruments to safely extract the contents of blackheads and whiteheads.
- Chemical Peels: This procedure involves applying a chemical solution, such as salicylic acid or glycolic acid, to the skin to exfoliate and unclog pores.
For Scarring and Post-Inflammatory Hyperpigmentation (PIH)
- Laser and Light-Based Therapies: A wide array of devices can be used to treat acne and its aftermath by reducing redness, resurfacing the skin to improve scar texture, and fading dark spots.
- Dermabrasion and Microdermabrasion: These are mechanical exfoliation techniques that remove the outer layers of skin, effective for shallow scars.
- Dermal Fillers and Subcision: For atrophic (depressed) scars, a dermatologist can inject dermal fillers to lift the base of the scar. Subcision is a technique where a special needle breaks the fibrous bands that tether the scar down.
The Blueprint for Clear Skin: Daily Routines and Lifestyle Integration
Effective medical treatment is only one part of the equation. A consistent, well-formulated daily skincare routine and mindful lifestyle choices are essential. The guiding principle for adult acne-prone skin is a gentle, supportive approach; harsh scrubs and stripping cleansers can compromise the skin's protective barrier and make acne worse.
The Foundational Skincare Routine for Acne-Prone Adult Skin
Morning Routine (Focus: Protection & Prevention)
- Gentle Cleanse: Start with a mild, non-abrasive, sulfate-free cleanser.
- Treatment Serum (Optional): An antioxidant serum with Vitamin C can help protect the skin and brighten post-acne marks. A serum with niacinamide can calm redness and regulate oil.
- Moisturize: Apply a lightweight, oil-free moisturizer labeled "non-comedogenic" (meaning it won't clog pores).
- Sunscreen: This is the most critical and non-negotiable step. Apply a broad-spectrum sunscreen with an SPF of 30 or higher every day.
Evening Routine (Focus: Treatment & Repair)
- Double Cleanse (If Applicable): If makeup or sunscreen was worn, start with an oil-based cleanser to dissolve it, followed by a gentle, water-based cleanser.
- Apply Prescription/Active Treatment: This is the ideal time to apply topical retinoids (adapalene, tretinoin), benzoyl peroxide, or azelaic acid to the entire affected area.
- Moisturize: Finish with a non-comedogenic moisturizer to buffer potential irritation and support the skin's barrier.
Best Practices in Depth: Cleansing, Moisturizing, and Sun Protection
- Cleansing: The goal is to clean the skin without stripping it. Use fingertips and lukewarm water.
- Moisturizing: The idea that acne-prone skin doesn't need a moisturizer is a harmful myth. When skin becomes dry, it may overproduce oil to compensate, leading to more breakouts. A non-comedogenic moisturizer provides necessary hydration and helps the skin tolerate active medications.
- Sun Protection: Sun exposure does not improve acne in the long term. It damages the skin, triggers inflammation, and significantly darkens post-inflammatory hyperpigmentation. Daily, year-round use of a broad-spectrum, non-comedogenic sunscreen is indispensable.
Beyond the Bathroom Sink: Lifestyle Modifications for Skin Health
- Stress Management: Incorporating stress-reduction techniques like meditation, yoga, or deep-breathing exercises can help lower cortisol levels and reduce inflammation.
- Sleep Hygiene: A consistent lack of quality sleep (less than 7-9 hours per night) can disrupt hormonal regulation and exacerbate acne.
- Product Selection: Scrutinize the ingredient lists of skincare, makeup, and hair care products. Opt for products labeled "non-comedogenic," "oil-free," or "won't clog pores."
- Hands Off: It is imperative to resist the urge to touch, pick, squeeze, or pop blemishes. This habit introduces bacteria, worsens inflammation, and is a primary cause of permanent scarring.
Navigating Your Journey: Professional Guidance and Psychological Well-being
The path to clear skin can be challenging, and it is important to recognize when self-management is no longer sufficient and professional expertise is required.
When to See a Dermatologist
Consulting a board-certified dermatologist is crucial under the following circumstances:
- Ineffective OTC Treatment: If over-the-counter products have not yielded significant improvement after a consistent 2-3 month trial.
- Severe or Scarring Acne: If breakouts consist of deep, painful nodules and cysts, or if any type of acne is beginning to leave scars.
- Significant Emotional Distress: If acne is causing feelings of depression, anxiety, or social withdrawal.
- Suspicion of an Underlying Condition: If acne is accompanied by other symptoms such as irregular periods or excess facial hair, it may be a sign of a hormonal disorder like PCOS.
- Need for an Accurate Diagnosis: Several other skin conditions can mimic acne, including rosacea and perioral dermatitis.
The Psychosocial Burden of Acne: It's Not Just Skin Deep
The impact of adult acne on mental health cannot be overstated. Research has consistently shown a strong correlation between acne and significant psychological distress. One study found that 96% of acne sufferers felt depressed about their condition, with 46% developing self-esteem issues and 31% actively avoiding social situations. Acknowledging this connection is a vital part of the healing process. Seeking medical treatment for acne is a form of comprehensive self-care that addresses both physical and mental well-being.
Conclusion: A Long-Term Strategy for Resilient Skin
The journey of managing adult acne is often a marathon, not a sprint. The evidence overwhelmingly shows that it is a complex, chronic medical condition influenced by an intricate web of hormonal, genetic, and environmental factors—not a personal or hygienic failing.
The key principles for successful long-term management are rooted in a multi-faceted strategy. This involves embracing a consistent, gentle daily skincare routine; utilizing targeted medical treatments guided by a dermatologist; and integrating mindful lifestyle choices that address internal triggers like stress and diet.
Patience and persistence are paramount. It can take at least two to three months of consistent treatment before noticeable improvements are seen. However, with a comprehensive, evidence-based plan tailored to individual needs, controlling adult acne and restoring confidence in one's skin is an achievable and worthwhile goal.
References
- American Academy of Dermatology.
- Collier, C. N., Harper, J. C., Cafardi, J. A., Cantrell, W. C., Wang, W., Foster, K. W., &Elewski, B. E. (2008). The prevalence of acne in adults 20 years and older. Journal of the American Academy of Dermatology, 58(1), 56-59.
- https://sylvaia.com/why-are-you-still-breaking-out-a-guide-to-adult-acne/
